Applicability of Artificial Intelligence in Healthcare in Resource-Poor Settings
Ashveena Gajeelee & Mansa Shroff
Abstract
This article focuses on institutional and resource constraints that have held back innovation and the scaling up of Artificial Intelligence (AI) in many Low and Middle Income Countries (LMICs). Given the proper infrastructure, AI-driven interventions hold promising transformations for public health in resource-poor countries. The results confirm the potential of startups implementing AI in resource poor settings such as Asia and Africa. Additionally, it highlights several prerequisites to a robust healthcare system: clarity in policies and regulations, well-defined roles and responsibilities of government bodies, political stability, and high investment in primary healthcare. Data collected and literature review on AI companies in LMICs are widely published. To gain deeper insights on current challenges in adoption and implementation of AI, we interviewed healthcare startups in LMICs that have the potential for a global outreach.
……
High-income countries are already benefiting from integrating Artificial Intelligence (AI) into their healthcare ecosystems, including analyzing big data, generating a more accurate diagnosis, and establishing a correlation between behavioral patterns and treatments. 1
Evidence shows that there is a strong relationship between technological innovation indicators and public health indicators. 2 In addition to saving lives, data integration allows for increased patient satisfaction, access to healthcare, and productivity of institutions. However, significant inequities exist. The COVID-19 pandemic has shed light on existing inequalities across countries and threatens to regress the health system by preventing access to quality healthcare.
The large volume of data generated and catalyzed by the COVID-19 pandemic has created a plethora of opportunities for applying AI to transform public health in resource-poor countries. AI-driven interventions are concentrated in four categories: diagnosis, mortality and morbidity risk assessment, disease outbreak and surveillance, and health policy and planning. 3 Most recently, countries have used AI to mitigate the spread of diseases and pandemics—from the Zika outbreak to Ebola and COVID-19. During the pandemic, India showed an increase of 45% in the use of AI. 4
The World Health Organization (WHO) is on a mission to achieve universal health coverage (UHC) by 2030 and transform healthcare through the use of AI and has advised countries to think of a national strategy to define the use of Big Data. The key areas of such a strategy would include the ethical use of data, governance and patients’ privacy, and a regulatory framework for sharing of health data across borders. Few countries have a patient-centric approach to using AI in their health system. 5 They tend to look into the ethical and governance framework ex post facto instead of as a guide to building the legal and regulatory framework.
The technical challenges are, of course, many. 6 For countries to have efficient use of AI in their public health systems, there are four core criteria they need to have: first, reliable, timely, cross-sectoral, and quality data as a feeder into decision-making and policy formulation; second, established AI technology to collect and mine these data from traditional sources as well as new ones (e.g., phone apps); third, the efficient training of personnel involved in the collection and analysis of data and maintenance of the technology; and finally, a strong and efficient regulatory framework that integrates global standards to allow for a smooth cross-border use of data. 7 However, these building blocks to the successful integration of AI integration in health systems require heavy and strategic investment and must also be accompanied by a thorough evaluation of the ethical implications of policies and strong political leadership.
The Data Dilemma
Healthcare data in LMICs are not scarce. Over the past decades, countries have had to implement monitoring and evaluation systems driven by reporting and accountabilities of donor agencies and international organizations. Subsequently, access to healthcare data has significantly improved, although there is still no central database that allows for easy analysis and understanding of the impact policy decisions have on health indicators. In the first-ever WHO global assessment of country data and health information systems released in 2021, 59% of countries were reported to have a well-developed or sustainable capacity for using data to drive policy and planning, but only 42% of countries had a good capacity for data access and sharing. 8
Countries like India and South Africa are already a good repository of data. This rise of the data economy is attracting startups, including Indian-based companies such as Niramai and Aindra (Table 1). Both of these companies have concentrated their investments in AI-powered tools in an effort to increase the early detection of breast and cervical cancer. Niramai offers innovative low-cost, non-invasive, and radiation-free breast cancer screenings that have now been integrated in 25 cities in India. 9 Aindra’s AI platform Astra is also built to detect cancer, particularly cervical cancer. These two forms of cancer lead mortality rates both in India and globally. 10
However, startups tend to operate and generate AI solutions from primary data often collected by skilled labor. While there is no doubt that the data is collected on a regular basis in many countries, data collection is often paper-based, and quality checks are not necessarily built in the process of computation. 11 The absence of interoperability also limits access and exchange of data among hospitals, research institutions, and policy makers, therefore preventing value-based healthcare. 12,13 Until countries create well-thought-out and integrated processes and systems that enable analyses and access to the data, LMICs will be stuck in the cycle of generating data but not optimizing it for medical use. 14
The Heavy Lifting: Legal, Governance, and Regulatory Frameworks That Work for LMICs
The building block to an AI-based healthcare system is a strong legal and regulatory framework that fosters entrepreneurship and innovation, data mining, and protection of patients' rights and privacy. Regulatory and legal frameworks for health data are generally weak in LMICs, and many issues remain at the forefront of ethical boundaries. There is no clear oversight of who has access to individual data, how these data are being used, and how ethically they have been gathered and used. These hurdles are further accentuated by the difficulty in localizing the data, since LMICs tend to have siloed health systems with minimum or no coordination among institutions. Smaller countries like Tanzania are trying to address this gap by moving towards a comprehensive data management system connecting government health institutions and the private sector. 15
A responsible use of AI in healthcare requires informed consent from the patient. The key hurdles to scaling up such cutting-edge efforts remain inaccessibility to reliable data, complex and unclear compliance requirements, and lack of protection for patients’ privacy and personal data. 16 The adoption of patient privacy laws has seen a steady growth but remains still low, with 55% of LMICs having legislation to protect the privacy of electronically held patient data and 34% covering sharing of health-related patient data between local healthcare professionals. 17 However, a strong regulatory framework is one that will not only look at the protection of patient data but also cross border data exchange, define the role of institutions and alignment of government bodies, and consolidate the business environment for the e-health industry to flourish. AI technology’s power is in big data analytics, such as the number of patient scans or mammography. Niramai (India) and HearX (South Africa), like many other technology companies, faced different regulations and compliance requirements for trials which are cumbersome and costly in scaling up. 18
Concerns have been raised about the governance of AI in healthcare. 19 These include the transfer of biases, lack of transparency and the black boxes of AI software, protection of individual privacy, and safety and liability issues with AI applications in clinical environments. Whether the government should be part of this regulatory framework versus a self-regulating system implemented at the industry level is highly debated as some fear a stifling of innovation and growth in the AI startup world. 20,21
The healthcare industry has a lot to gain from the lessons learned from the financial crisis of 2008, when regulatory institutions were severely criticized for not ensuring appropriate and timely reporting on financial instruments. Regulators should ensure faster processes for regulatory approval of AI solutions which need to be timely, flexible, and often global. 22 The most relevant lesson from the financial crisis is the need for coordination and synergy between regulators and the private sector. Almost all the start-ups that were interviewed shared a common difficulty in fundraising or the lack of support from key stakeholders in the healthcare systems such as insurance companies. The massive investment required to develop the AI platforms in the constantly evolving environment, the cost of regulatory compliance, and the training of personnel often deter start-ups from scaling up.
A Radical Rethinking of Healthcare in LMICs
With the WHO developing the World Health Data Platform to create a unified, modern end-to-end central repository for all health data, there is a great potential for artificial intelligence to increase access to affordable healthcare. 23 AI technology will alleviate the lack of healthcare professionals by allowing remote diagnosis, collection of local disaggregated data, and a business model that can decrease the cost of healthcare. 24 However, many structural issues need to be addressed: access to the internet, a system to support entrepreneurship and innovation, an education system that fosters coding and AI expertise, open access to data, system interoperability, and a policy and regulatory framework that enables business development. 25
The COVID-19 crisis has ushered us into a new era of AI in healthcare that requires a radical rethinking of service delivery in LMICs. 26 Low- and no-touch services are now necessary for patients—typically at the highest risk for COVID-19 morbidity and mortality due to their age—to access medical care. 27 We cannot afford another pandemic or health crisis. In the wake of the World Health Assembly, world leaders must put aside their political differences, or we may have to forgo the significant benefits of health technology for humanity.
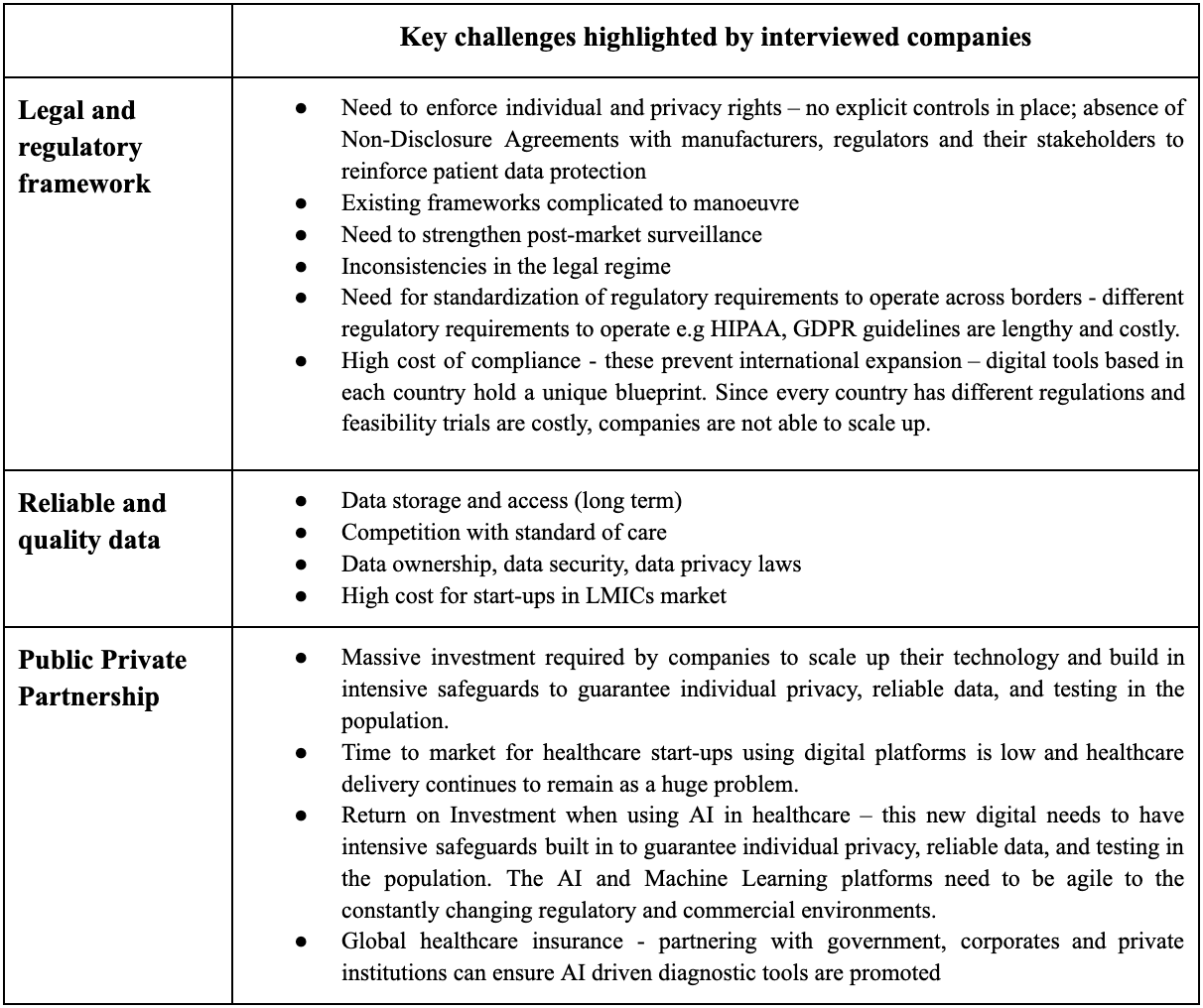
Table 1: Main challenges to scaling up by AI-powered health companies in LMIC
Acknowledgements
Cherie Lynn Ramirez, Dr. Amit Gajeelee
Interviewees
mPedigree: Daniel Kwakye and Selorm Branttie
HearX: De Wet Swanepoel
Niramai: Geetha Manjunath
Aindra: Adarsh Natarajan
References
- El Bcheraoui C, Weishaar H, Pozo-Martin F, Hanefeld J. Assessing COVID-19 through the lens of health systems’ preparedness: time for a change. Globalization and Health. 2020 Nov 19;16(1).
- How to build a better health system: 8 expert essays [Internet]. World Economic Forum. Available from: https://www.weforum.org/agenda/2020/10/how-to-build-a-better-health-system/
- Noorbakhsh-Sabet N, Zand R, Zhang Y, Abedi V. Artificial Intelligence Transforms the Future of Health Care. The American Journal of Medicine. 2019 Jul;132(7):795–801.
- Ellahham S, Ellahham N, Simsekler MCE. Application of Artificial Intelligence in the Health Care Safety Context: Opportunities and Challenges. American Journal of Medical Quality [Internet]. 2019 Oct 4;35(4):106286061987851.
- Ethics and governance of artificial intelligence for health: WHO guidance. Geneva: World Health Organization; 2021. Licence: CC BY-NC-SA 3.0 IGO
- Gill P. Technological innovation and its effect on public health in the United States. Journal of Multidisciplinary Healthcare. 2013 Jan 31.
- Schwalbe N, Wahl B. Artificial intelligence and the future of global health. The Lancet. 2020 May;395(10236):1579–86.
- SCORE for health data technical package: global report on health data systems and capacity, 2020 [Internet]. www.who.int. [cited 2022 Oct 27]. Available from: https://www.who.int/publications/i/item/9789240018709
- Niramai’s solution to screening breast cancer? A low-cost device. The Economic Times [Internet]. [cited 2022 Oct 27]; Available from: https://economictimes.indiatimes.com/tech/startups/niramais-solution-to-screening-breast-cancer-a-low-cost-device/articleshow/79415822.cms
- AI for affordable cervical cancer screening [Internet]. website. [cited 2022 Oct 27]. Available from: https://indiaai.gov.in/case-study/ai-for-affordable-cervical-cancer-screening
- Wyber R, Vaillancourt S, Perry W, Mannava P, Folaranmi T, Celi LA. Big data in global health: improving health in low- and middle-income countries. Bulletin of the World Health Organization. 2015 Jan 30;93(3):203–8.
- Dash SP. The Impact of IoT in Healthcare: Global Technological Change & The Roadmap to a Networked Architecture in India. Journal of the Indian Institute of Science. 2020 Oct;100(4):773–85.
- Ndabarora E, Chipps JA, Uys L. Systematic review of health data quality management and best practices at community and district levels in LMIC. Information Development. 2013 Jun 27;30(2):103–20.
- Maina J, Ouma PO, Macharia PM, Alegana VA, Mitto B, Fall IS, et al. A spatial database of health facilities managed by the public health sector in sub Saharan Africa. Scientific Data [Internet]. 2019 Jul 25;6(1). Available from: https://www.nature.com/articles/s41597-019-0142-2
- Nsaghurwe A, Dwivedi V, Ndesanjo W, Bamsi H, Busiga M, Nyella E, et al. One country’s journey to interoperability: Tanzania’s experience developing and implementing a national health information exchange. BMC Medical Informatics and Decision Making. 2021 Apr 29;21(1).
- mPedigree. Kenya’s e-Health Department has begun piloting a system to curb fake goods [Internet]. Mpedigree.com. [cited 2022 Oct 3]. Available from: https://mpedigree.com/news/kenyas-e-health-department-has-begun-piloting-a-system-to-curb-fake-goods-2/
- Report of the third global survey on eHealth Global Observatory for eHealth Global diffusion of eHealth: Making universal health coverage achievable [Internet]. Available from: https://apps.who.int/iris/bitstream/handle/10665/252529/9789241511780-eng.pdf?sequence=1
- Swanepoel DW, Olusanya BO, Mars M. Hearing health-care delivery in sub-Saharan Africa--a role for tele-audiology. J Telemed Telecare [Internet]. 2010 [cited 2022 Oct 3];16(2):53–6. Available from: https://pubmed.ncbi.nlm.nih.gov/20008052/
- Reddy S, Allan S, Coghlan S, Cooper P. A governance model for the application of AI in health care. Journal of the American Medical Informatics Association [Internet]. 2019 Nov 4;27(3). Available from: https://academic.oup.com/jamia/advance-article-abstract/doi/10.1093/jamia/ocz192/5612169
- Jones E, Knaack P. Global Financial Regulation: Shortcomings and Reform Options. Global Policy [Internet]. 2019 Feb 18;10(2):193–206. Available from: https://onlinelibrary.wiley.com/doi/full/10.1111/1758-5899.12656
- S C Rajeev, Ministry of Health & Family Welfare, Government of India. Placing the draft of “Digital lnformation Security in Healthcare, act (DISHA)” in public domain for comments/views [Internet]. 2017. Available from: https://www.nhp.gov.in/NHPfiles/R_4179_1521627488625_0.pdf
- Fanelli S, Salvatore FP, De Pascale G, Faccilongo N. Insights for the future of health system partnerships in low- and middle-income countries: a systematic literature review. BMC Health Services Research. 2020 Jun 22;20(1).
- WHO Integrated Data Platform, [Internet]. website. [cited 2022 Nov 6]. Available from: https://www.who.int/tools/who-integrated-data-platform
- Swanepoel D. The International Classification of Health Interventions (ICHI) – a new tool for describing and reporting interventions in audiology [Internet]. Taylor & Francis. 2022 [cited 25 September 2021]. Available from: https://www.tandfonline.com/doi/full/10.1080/14992027.2020.1736344
- Feijóo C, Kwon Y, Bauer JM, Bohlin E, Howell B, Jain R, et al. Harnessing artificial intelligence (AI) to increase wellbeing for all: The case for a new technology diplomacy. Telecommunications Policy. 2020 Jul;44(6):101988.
- Yousuf Hussein S, Wet Swanepoel D, Biagio de Jager L, Myburgh HC, Eikelboom RH, Hugo J. Smartphone hearing screening in mHealth assisted community-based primary care. J Telemed Telecare [Internet]. 2016 [cited 2022 Oct 3];22(7):405–12. Available from: https://pubmed.ncbi.nlm.nih.gov/26468215/
- Wahl B, Cossy-Gantner A, Germann S, Schwalbe NR. Artificial intelligence (AI) and global health: how can AI contribute to health in resource-poor settings? BMJ Glob Health [Internet]. 2018 [cited 2022 Oct 3];3(4):e000798. Available from: https://pubmed.ncbi.nlm.nih.gov/30233828/